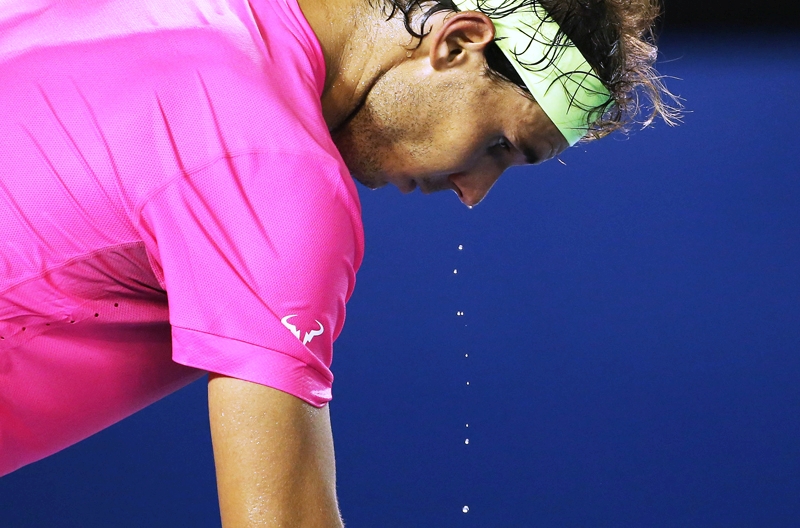
The heat of the moment: safety first!
Heat-related illness in athletes can have potentially catastrophic consequences. SPB looks at the best-practice evidence for assessing risk and preventing illness this summer
When it comes to life-threatening conditions associated with sport participation, sudden cardiac arrest and concussion probably spring to mind. However, although less publicised, heat stroke and heat-related illness is equally serious. Data shows that when heatwaves occur, overall mortality is increased across all segments of the population, mainly as a result of complications such as respiratory failure and myocardial infarction(1). However, what is less well known is that the incidence of heat-related illness is highest among men aged 15 to 19 years and is most often associated with athletic activities(2).To complicate things further, cases of heat stress tend to be handled on a case-by-case basis rather than by being addressed collectively as a public health concern. In the US, The National Institute for Occupational Safety and Health initiated heat stress criteria regarding worker heat stress safety in 1986, yet in even now, few people are aware of these criteria, of the risk factors associated with a predisposition to heat stress, or of the signs or symptoms to look for that represent risk factors for heat stress(3).
Temperature regulation
Heat stress/illness occurs when the body is no longer able to maintain its temperature equilibrium and core temperature rises sufficiently to interfere with other physiological processes. There are a large number of factors that will determine if and when heat stress will strike any particular athlete. These include environmental factors (temperature of the environment, humidity levels, wind chill), the age, gender and cardiovascular fitness of the athlete and even any medications (see table 1) they take(4). Overall however, tolerance to dehydration is more robust when individuals are physically fit and young, while the ability to adapt to heat declines with age, poor fitness levels and the presence of disease.Table 1: Medications and heat stroke risk(8)
Substance Mechanism of interference with temperature
homeostasis
LegalAlcohol HR decrease, plasma volume depletion
Amphetamines HR increase, increase in sweating
Anticholinergics HR lability, abnormal sweating
Antihistamines HR lability, abnormal sweating
Antihypertensives HR lability
Benzodiazepine HR lability, abnormal sweating
Calcium channel blocker HR lability, venous pooling, abnormal sweating
Diuretics Plasma volume depletion, decreased vasodilation
Laxatives HR lability, abnormal vasodilation
Neuroleptics HR lability, abnormal sweating
Phenothiazine Electrolyte imbalance
Topiramate Electrolyte imbalance
Tricyclic antidepressants Electrolyte imbalance
Illegal
Cocaine HR increase, increased sweating
Phencyclidine (PCP) Abnormal temperature regulation
Lysergic acid diethylamide (LSD) HR lability, abnormal sweating
NB: ‘HR’ indicates heart rate
The type of clothing worn plays a major role in influencing the ability to maintain safe core temperatures and adjust to extreme environmental heat. Indeed, the wrong or excessive clothing can be extremely important in determining whether athletic heat exhaustion and heat stroke mortality occur(5). The exercise workload is also critical – the higher the workload, the greater the amount of heat needs to be dissipated in order to maintain a stable core temperature. In addition to hydration status, fluid replacement before during and after exercise is also a critical factor; under normal conditions (ie in the absence of disease, medications and other complicating factors), the human body can maintain a stable core temperature even when stressed by extreme environmental temperatures as long as adequate hydration is continuously provided(6,7). However, while maintaining adequate hydration sounds straightforward in principle, the practice can be much more challenging for both athletes and trainers/coaches alike – see box 1).
Box 1: Hydration fundamentals
A comprehensive hydration strategy entails ensuring good hydration before training/competition, maintaining hydration as far as possible during training/competition and then ensuring that any shortfall is fully replaced as soon as possible afterwards. Fluid loss via urine and especially via sweating involves the loss of electrolyte minerals – calcium, magnesium, sodium, potassium and chloride. Although the composition varies from person to person, a litre of sweat typically contains around the following(9,10):Mineral Grams (g)
Calcium 0.02g
Magnesium 0.05g
Sodium 1.15g
Potassium 0.23g
Chloride 1.48g
Replacement of these minerals in an electrolyte mineral containing drink is desirable because while the amounts of these minerals lost during sweating is generally small compared to total body stores, prolonged heavy sweating can lead to significant losses (particularly of sodium), which has been associated with undesirable side effects such as cramping. Drinking lots of pure water effectively dilutes these concentrations of electrolyte minerals, which can lead to an impairment of a number of normal physiological processes. An extreme example of this is hyponatraemia, where low plasma sodium levels disrupts the dynamics of water exchange (osmotic balance) across the blood-brain barrier, causing symptoms such as confusion, seizure, coma and even death.
Another reason is that drinks containing added sodium have been shown to help the physiological drive to drink, therefore stimulating a greater voluntary intake of fluid compared to plain water(11). In addition, when the electrolyte minerals (in particular sodium) are present at the appropriate concentrations, the rate of fluid absorption from the small intestine appears to be enhanced, especially in conjunction with small amounts of glucose(12). This is especially important where the rapid uptake of fluid into the body is important, for example ingesting fluid to maintain hydration during exercise.
Screening for heat stroke risk
The principles of temperature regulation outlined above are easy enough to understand. However, what’s far trickier is to determine the risk of heat stroke for any one individual at any given time - yet this is exactly what sports medicine personnel, coaches and trainers need to be able to do in order to keep athletes safe and well in hot conditions. One approach is to use data on environmental variations in temperature, humidity, and radiation as well as the individual’s heart rate and aerobic tolerance and combine this in a formula to give a ‘heat stress risk’ score. One such formula incorporates both environmental factors (environmental stress index - ESI) and personal factors (personal stress index - PSI) and uses them in the following formula in box 2 below(13):Box 2: Formula for calculating heat stress index(13)
This heat stress risk formula is as follows:ESI = 0.63Ta – 0.03RH + 0.002SR + 0.0054 (Ta × RH) – 0.073(0.1 + SR)–1
PSI = 5(Tret – Tre0) × (39.5 – Tre0)–1 + 5(HRt – HR0) × (180 – HR0)–1
In this formula:Ta = ambient temperature
RH = relative humidity
SR = solar radiation
Tre0 = initial rectal temperature
Tret = rectal temperature after time t
HR0 = initial heart rate
HRt = heart rate after time t
The PSI and ESI values obtained by this formula are designed to reflect cardiovascular strain on the individual relative to the environmental stress on a scale between 0 and 5. The higher the value obtained, the higher the strain. Importantly, the use of this formula and coordination of work-rest cycles in training have successfully been used to prevent the risk of future heat stress injuries in military recruits. One limitation of this type of risk assessment is the need to measure rectal temperature, which is invasive - also and the need for specific meteorological equipment to measure the strength of solar radiation and relative humidity.
Which athletes are at risk?
The first step in reducing the risk of heat stroke is recognize which athletes are most likely at risk and when. Athletes at risk for heat stress include all those whose typical workloads are high and whose events/training takes place in warm indoor or outdoor conditions (where direct heating from solar radiation is also a potential problem). In reality, this includes distance runners, soccer players, hockey players, triathlon competitors, weight-lifters, boxers etc. Cyclists can be at risk in very hot conditions but the risk is generally lower than in runners because of the cooling effects generated by moving through the air at relatively high speeds. It’s also worth adding that athletes with learning disabilities may be at proportionately higher risk because they might find it harder to absorb the information about and put into practice the guidelines on regular drinking during exercise. These athletes will benefit from more frequent rest cycles and regular prompting from coaches to drink fluid.The workload undertaken is also important. All other things being equal, for any given individual, the higher the workload, the greater the risk of heat stress in that individual. Across different individuals, the fitter the individual, the lower the risk of heat stress in that individual. In addition to the use of heat stress risk formulae, what other tools can and should be used prior to training athletes in the heat? According to Dr Lilly Ramphal-Naley, a US expert in preventative medicine, the use of a medical questionnaire to assess cardiopulmonary function, fitness level, prior episodes of heat stress, and medications is most definitely desirable. In addition, a pre-exercise assessment of blood pressure and BMI should also be carried out, and for those who expect to be working at higher intensities, other pre-exercise tests such as electrocardiograms (EKG), step tests and even exercise stress tests may be warranted. Table 2 (below) sums up these recommendations.
Table 2: Recommendations for heat stress screening for workers and athletes(3)

Screening
Cardiac screening tests such as a stress echocardiogram are considered as the gold standard for cost-effective screening in order to discover whether someone could be susceptible to the physiological stresses of exercising in a hot environment(14). However, this kind of testing is expensive and time-consuming and given that young athletes with no history of cardiac problems are at very low risk, tests such as stress echocardiograms are better reserved for an athlete over 35 who is either a) intending to participate in medium to high-intensity exercise or b) whose medical questionnaire shows that he/she has cardiac risk factors. The age demarcation of 35 years arises from the fact that once this age is reached, cardiovascular system begins to show age-related changes, resulting in an increased risk of unpredictable and undesirable cardiovascular complications.Another category of athlete that deserves special mention in this context is the diabetic. Diabetes is a known cardiac risk factor; recent research shows that diabetes is highly associated with ischemic heart disease and stroke, and also that these kinds of events are more likely to occur when an individual is exposed to heat stress(15). A medical screening questionnaire can determine whether diabetes is present and if so, more thorough screening can be implemented before an athlete exercises in the heat. However, many people with diabetes (including athletes) may be oblivious to their condition, especially in the early stages. Data gathered last year by the International Diabetes Federation suggests that as many as 183 million people globally (around half of those who have diabetes) are unaware of the fact. Given these facts, the safe option for those with athletes in their care is to carry out routine screening for the presence of diabetes before subjecting them to heat stress.
Medical questionnaires
As can be seen from table 2 and the discussion above, the implementation of some kind of pre-exercise medical screening to assess heat stress risk in the form of a questionnaire is always desirable in athletes, regardless of age or fitness. Screening athletes using pre-participation physical examinations (PPEs) can help health care professionals and coaches identify predisposing factors of exertional heat illnesses and identify those at risk. Typically, the PPE includes an evaluation of general medical considerations and orthopaedic injuries; however, evidence suggests that athletic trainers would be better equipped to prevent heat stress illness with more information about any previous history of cardiovascular, respiratory, and heat illnesses(16-18).The intrinsic risk factors for exertional heat illnesses include a previous episode of heat illness, poor cardiovascular and physical fitness, inadequate heat acclimatization, dehydration or electrolyte imbalance, recent febrile illness, sleep deprivation, a ‘never give up’ or ‘warrior’ mentality, an unusually high level of motivation or zealousness and use of questionable drugs or herbal supplements. Many of these factors can be identified during a PPE but current research supports extending the scope of the PPE to include more indicators for cardiovascular, respiratory, and general medical conditions, including exertional heat illnesses(16-20). In a key study, researchers identified some key questions that should be asked as part of a PPE in order clarify the intrinsic risk factors and further identify those athletes who might be at particular risk(21). These are shown below in table 3.
Table 3: Key questions to determine intrinsic risk of exercise-related exertional heat illness

According to the researchers, when combined with the information gathered from a PPE, these questions could help to determine those at particular risk of exertional heat illness and who might otherwise slip through the net. This in turn could allow a more accurate ‘heat stress risk score’ to be obtained, resulting in more effective adjustments to training in order to ensure athletes avoid heat stress/illness.
Summary
Heat stress and heat illness during exercise can lead to serious health complications in athletes and in the most serious cases, can be fatal. Moreover, the evidence suggests that this risk may be underestimated by some coaches, athletic trainers and healthcare practitioners. In addition to identifying the environmental heat loading, it’s extremely important to assess each athlete’s vulnerability to heat stress/illness. This requires consideration of a large number of factors, including medications, medical history, lifestyle factors, training history, cardiovascular fitness index. This information should be considered an essential part of any pre-participation physical examination to determine heat stress/illness risk and keep athletes safe.References
- Environ Health 2009;8:40
- MMWR Morb Mortal Wkly Rep 2011;60(29):977– 980
- Baylor University Medical Center Proceedings July 2012; Vol25 (3)
- Glob Health Action 2010;3.
- Occup Med 1990;5(1):79–91
- Scand J Med Sci Sports 2010;20(Suppl 3):117–124
- J Occup Med Toxicol 2008;3:21
- Am Fam Physician 2005;71(11):2141– 2142
- Geigy Scientific Tables, 8th Ed, Ciba-Geigy Ltd. 1981
- Human Physiology, 2nd Ed, Springer-Verlag, Berlin. 1989
- Amer. J. Physiol. 258 (Gastrointest. Liver Physiol.) 21: G216-G222, 1990
- Res Quart 51: 299-305, 1980
- J Basic Clin Physiol Pharmacol 2003;14(1):17–30
- Am Heart J 2011;161(5):900–907
- Cardiovasc Diabetol 2011;10:86
- J Adolesc Health. 1992;13(suppl 2):1S–65S.
- JAMA. 1998;279(22):1817–1819.
- Pediatrics.1980;66(5):736–745
- Clin Cornerstone. 2001;3(5):10–25.
- Cleve Clin J Med. 2004;71(7):587–597.
- Journal of Athletic Training 2011;46(2):176–184
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Performance Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Keep up with latest sports science research and apply it to maximize performance
Today you have the chance to join a group of athletes, and sports coaches/trainers who all have something special in common...
They use the latest research to improve performance for themselves and their clients - both athletes and sports teams - with help from global specialists in the fields of sports science, sports medicine and sports psychology.
They do this by reading Sports Performance Bulletin, an easy-to-digest but serious-minded journal dedicated to high performance sports. SPB offers a wealth of information and insight into the latest research, in an easily-accessible and understood format, along with a wealth of practical recommendations.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Performance Bulletin helps dedicated endurance athletes improve their performance. Sense-checking the latest sports science research, and sourcing evidence and case studies to support findings, Sports Performance Bulletin turns proven insights into easily digestible practical advice. Supporting athletes, coaches and professionals who wish to ensure their guidance and programmes are kept right up to date and based on credible science.









