You are viewing 1 of your 1 free articles. For unlimited access take a risk-free trial
Cycling back pain: blame the bike?

Highlighting recent research, Andrew Hamilton explains why cyclists suffering from chronic low-back pain should look inwards before blaming their bike
Cycling is rightly regarded as a low-injury risk sport by virtue of the smooth nature of the pedalling action and absence of jarring impact forces. If you’ve never been affected by lower back pain while riding, it might surprise you to learn that chronic lower back pain (CLBP) among cyclists is surprisingly common - some studies have shown that among pro cyclists, as many as 35% will suffer a lower back injury in any one year. For cyclists with low back pain, the situation is further complicated by the fact that very few studies into this problem have been carried out. Those that have been carried out, have tended to focus on factors relating to the bike set up such as bike and frame geometry – eg is the cyclist trying to force his/her body to fit a bike that is inherently unsuitable? However, a fascinating study by Dutch scientists suggests that for many cyclists with CLPB, the problem lies not with the bike but within(1).Are you sitting comfortably?
In this study, 17 recreational and competitive cyclists were asked to perform a 2-hour bike ride using their own personal racing bikes. Eight of these cyclists suffered from non-specific CLBP while the other nine (matched for age and gender) reported no lower back problems. During this ride, each cyclist had the movement patterns in their lower back region analysed using a wireless system, which recorded data and sent it wirelessly to the researchers in the lab. The researchers then asked each cyclist to report how much lower back pain they had experienced both during and after the ride, and compared this with the measurements taken during the ride.Flexed back posture
When the data from the cyclists with CLBP was compared with that from the symptom-free cyclists, it became apparent that the movement patterns were significantly different between the two groups. The CLBP cyclists were more flexed (more rounded in the lower back) throughout the ride compared to the pain-free cyclists. This more flexed lower back position was in evidence regardless of the saddle angle/position the cyclists were using. The CLBP cyclists also reported a significant increase in pain over the course of the 2-hour ride whereas the healthy cyclists reported no increase in discomfort.This study is interesting because it suggests that in cyclists who suffer from chronic low back pain during and after riding, an over-flexed lower back position when riding is far more likely than is observed in pain-free cyclists. As the researchers went onto explain: “This increased and sustained lower back flexion appears to reflect an inherent maladaptive (ie faulty) motor control pattern at the lower lumbar spine during cycling.” In other words, while bike set up still matters, for many cyclists who suffer CLBP, the problem lies within – specifically the way lower back posture is maintained (or not) when riding.
Although there’s relatively little data on this topic in the literature, these findings do seem tie in with what other research into has been carried out. For example, studies have shown that the stabilising power of key core muscles in the lower back called multifidus (see figure 1) is reduced after just five minutes of static flexion – ie the position adopted while riding a bike(2). To make matters worse, the researchers also found that this static flexion led to spinal tissue ‘creep’, making it even harder for the lumbar stabilising muscles to function optimally.
Figure 1: Location of lumbar multifidus muscles
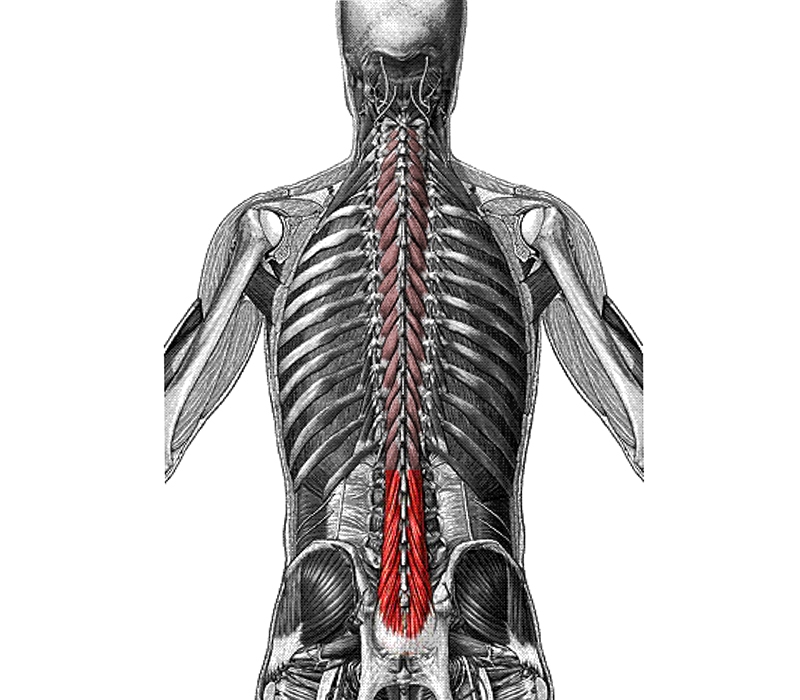
The lumbar multifidus muscles run deep to the lumbar spine and are shown highlighted in red.
Another study examined low-back musculature in cyclists with and without back pain(3). In this study, researched compare the thickness of lateral abdominal muscles and cross sectional area of lumbar multifidus spinae muscles of competitive off-road cyclists, with and without back pain. They also assessed the maximum isometric back strength and endurance, as well as flexibility. The results revealed that cyclists with low-back pain had a significantly lower thickness of transversus abdominis and cross-sectional area of lumbar multifidus. And while there were no differences in the lumbar flexibility or maximal strength of the subjects, the cyclists with lower-back pain showed reduced lower-back endurance when tested with repeated reps at 50% of maximum back strength.
Finally, the findings of a 2017 review study (a study that pools the all data from previous studies) also tends to confirm the above(4). In this study, researchers sought to establish what relationships exist between body positioning, spinal kinematics, and muscle activity in active cyclists with chronic lower back pain. Pooling the data from eight studies, the researchers found that increased lumbosacral flexion angle (forward bending) as a result of low handlebar height was a factor in low-back pain. However, the data also showed that core-muscle activation imbalances, and back extensor endurance deficits were very significant in determining whether cyclists were likely to suffer from low-back pain – ie intrinsic factors played a big role, not just bike set up.
Practical implications
The data on low-back pain causal factors in cyclists is quite sparse. However, from the research that has been carried out, we can conclude that while bike set up is a factor, other (intrinsic) factors may be more important. In terms of advice for cyclists, this doesn’t mean that bike set up should be ignored; on the contrary, ensuring your riding position and posture is optimized remains very important – especially handlebar height (for more in-depth information on this subject, see this Sports Performance Bulletin article). But once bike set up has been optimized, the obvious implication that follows is that in cyclists with persistent lower back pain, investigating rehabilitation and prevention strategies that address the control over the lower lumbar region during cycling (eg a programme of stretching and core strengthening) is the next logical step. Where this is the case, consulting a qualified physiotherapist (preferably with a background in cycling or experience of treating cyclists) is highly recommended!References
- Br J Sports Med. 2014 Apr;48(7):609
- Spine (Phila Pa 1976). 2009 Aug 1;34(17):1873-8.
- J Back Musculoskelet Rehabil. 2015;28(4):635-44
- Sports Health. 2017 Jan/Feb;9(1):75-79
Newsletter Sign Up
Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Keep up with latest sports science research and apply it to maximize performance
Today you have the chance to join a group of athletes, and sports coaches/trainers who all have something special in common...
They use the latest research to improve performance for themselves and their clients - both athletes and sports teams - with help from global specialists in the fields of sports science, sports medicine and sports psychology.
They do this by reading Sports Performance Bulletin, an easy-to-digest but serious-minded journal dedicated to high performance sports. SPB offers a wealth of information and insight into the latest research, in an easily-accessible and understood format, along with a wealth of practical recommendations.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Performance Bulletin helps dedicated endurance athletes improve their performance. Sense-checking the latest sports science research, and sourcing evidence and case studies to support findings, Sports Performance Bulletin turns proven insights into easily digestible practical advice. Supporting athletes, coaches and professionals who wish to ensure their guidance and programmes are kept right up to date and based on credible science.













