Low back pain: muscle timing matters for prevention

Recent research on muscle activation timing in the postural muscles of the trunk has implications for low back pain therapies in sportsmen and women...
Lower back pain (LBP) is a common condition among sportsmen and women (see box 1). However, as our understanding of the causes of back pain has progressed, so have the treatment and prevention approaches. An example of this has been the growing emphasis over the last 15 years on functional training for the postural muscles of the trunk – an approach to LBP treatment/prevention that is now fairly widely accepted among athletes, clinicians and trainers. However, while some research has highlighted benefits of this mode of training for people with back pain and for carrying out everyday activities, less research has been performed on the benefits of core training for injured athletes, and how this training should be carried out to optimize sporting performance.Box 1: Prevalence of low back pain in athletes
Low back pain (LBP) among sportsmen and women is a common phenomenon. How common of course depends on numerous factors such as the nature of the sport, the level of participation and previous injury history of the athlete concerned. For example, a Norwegian study found that LBP was more common among cross-country skiers and rowers than orienteerers and non-athletic controls(1). Among the cross-country skiers, 63% reported at least one episode of LBP during the previous 12 months – a higher figure than matched non-athletic controls. Among the rowers, 25.6% of subjects reported missing training because of low back pain over the same time period compared to just 13.7% of the orienteerers. All the athletes however reported more low back pain during periods when training and competition load was higher. Another study on triathletes indicated that the lifetime incidence of LBP was 67.8%, with 23.7% of cases possibly being related to degenerative changes in the spinal discs(2). The number of triathlons in which the respondents had participated and the presence of previous sports-related injuries were also predictive of the likelihood of LBP. Meanwhile, a study of the prevalence of lumbar disc degeneration in elite athletes with lower back pain at the Sydney 2000 Olympic Games showed that elite athletes were likely to have a greater prevalence and degree of lumbar disc degeneration than the normal population, leading to an increased risk of LBP(3).Core training and muscle activation
Many elite athletes undertake core stability and core strength training as part of their training program, despite contradictory findings and conclusions as to their efficacy. This is mainly due to the lack of a gold standard method for measuring core stability and strength when performing everyday tasks and sporting movements. A further confounding factor is that because of the differing demands on the core musculature during everyday activities (low load, slow movements) and sporting activities (high load, resisted, dynamic movements), research performed on sedentary patients may not apply equally to the sporting environment. This means that data regarding core training programs and their effectiveness for athletes is still relatively lacking.One aspect of postural muscle function that has received particular attention in recent years is muscle activation patterns – ie the precise way the muscle fibers are programmed to fire by nervous impulses sent from the brain. Understanding how a certain type of movement activates (or fails to activate) key postural muscles in the trunk needed for a healthy and stable spine is vital to unraveling the role of these postural muscles in trunk stabilization.
Much of the initial work in this area tended to focus primarily on the magnitude and sequence of electromyographic (EMG – patterns of electrical activity in muscles) activation in postural muscles, and this knowledge has proved invaluable to physiotherapists and sports physiologists seeking a better understanding of LBP. However, there’s also been a growing interest in the timing of such activity, and its relationship to LBP.
The ability to rapidly control the timing of core muscle contractions in response to an unexpected postural perturbation (eg a trip or trying to catch a falling object suddenly and without warning) is considered paramount for maintaining posture and balance, and therefore in promoting good lower back health. The studies carried out show that (compared with healthy controls), in addition to demonstrating reduced EMG activity, individuals with chronic LBP also demonstrate delayed activity response to both anticipated and unanticipated postural perturbations(4,5).
In plain English, when reacting to a sudden and unexpected movement, chronic back pain sufferers are slower in firing up the key core muscle fibers that are needed to stabilize the trunk. Moreover, research also shows that if you induce low back pain in otherwise healthy individuals, their muscle activity patterns are altered for the worse when carrying out tasks involving trunk flexion/extension (bending forwards/backwards), as well as performing reaching and rapid arm-movement tasks. In short, if you suffer from chronic LBP, your movement patterns are impaired in a way that makes you vulnerable to further injuries when carrying out simple tasks such as bending forwards or reaching out with your arms.
Timing and pain
One criticism of the kinds of studies used above was that the ‘real-life’ perturbations used to activate core muscles were not sufficiently realistic to enable meaningful ‘real-world’ conclusions to be drawn. However, a landmark study by Danish scientists examined postural responses in the presence of, full body perturbations, which were designed to be far more functionally relevant – ie better approximate real life(8). These perturbations were produced by a computer-controlled platform that allowed movement in three-dimensions to produce tilting or sliding movements closely resembling ‘tripping over an obstacle’ or ‘slipping on a wet surface’.In the study, the researchers assessed the activation of the erector spinae (deep low back stabilizers see figure 1) and external oblique muscles in response to unanticipated, postural perturbations before and after the induction of acute LBP in healthy individuals. Each experimental session consisted of a baseline, control, and an acute LBP condition. For the control and acute LBP condition, isotonic or hypertonic saline, respectively, was injected into the right erector spinae muscle. In each condition, participants stood on a moveable platform during which 32 randomized postural perturbations were performed. These consisted of 8 repetitions of four perturbation types performed over a period of 4–5 minutes including forward and backward slides and tilts. During these perturbations, muscle activation patterns were recorded from the erector spinae and external oblique muscles, as well as the subjective pain experienced by the subjects.
Figure 1: Location of the core-stabilizing multifidus muscles in the trunk
The lumbar multifidus muscles run deep to the lumbar spine and are shown highlighted in red.
The results showed that compared to the ‘no back pain’ condition (control), back pain delayed the onset time of both erector spinae and external obliques for the forward and backward sliding perturbations. It was also apparent that in the back pain condition, the EMG amplitude was reduced for all perturbations (see figures 2a-2d).
Figure 2: EMG findings
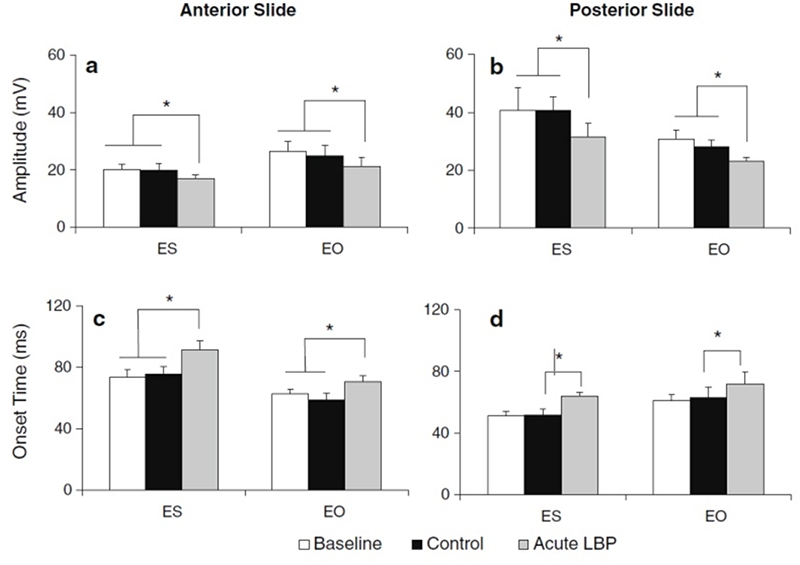
EMG amplitude (a, b) and onset time (c, d) of the erector spinae (ES) and external oblique (EO) during the baseline, control, and low back pain conditions for the anterior and posterior sliding perturbations(7).
The findings of the above Danish study appear to be supported by those from another study on altered electromyographic activation patterns in response to perturbations of standing balance(9). In this study, researchers evaluated the intermuscular patterns of EMG activations from 24 people with and 21 people without a history of chronic and recurrent LBP in response to twelve directions of support surface translations. The results of this experiment indicated that the subjects with LBP had dysfunctional patterns of activation of the erector spinae muscles – specifically in that, although they were slightly more activated in their resting state, they didn’t exhibit the expected burst of activity when faced with an unexpected perturbation.
Late onset muscle activation in athletes
The studies above looked at onset activation times in (otherwise) healthy but sedentary people. But what are the implications for athletes? Unfortunately, the literature in this respect is very thin on the ground. However, one study looked at the reflex response of superficial trunk musculature in athletes with chronic low back pain to see whether similar patterns of delayed muscle activation onset exist in the athletic body(10). In particular, the researchers sought to compare reflex response occurring between approximately within 40ms to 100ms in athletes with chronic LBP against asymptomatic athletes.To do this, 24 athletes with chronic LBP were compared with 25 asymptomatic athletes. In the standing positions, perturbations were introduced both expectedly and unexpectedly while the surface EMG of the rectus abdominis (abdominal) and erector spinae muscles were recorded. The delay in the onset of muscle activation and the amplitudes when the reaction did occur were compared between the two groups.
Compared to the pain-free athletes, muscle activation onset was delayed in the LBP athletes when the athlete experienced unexpected perturbations. However, during the expected perturbations, no change was observed. Another finding was that in the LBP athletes, the amplitudes of muscle activity were significantly lower in both tasks for rectus abdominis and in the expected task for erector spinae. The researchers went onto conclude that ‘the delayed muscle activation and amplitudes during the perturbation challenges could predispose athletes to recurrent low back pain and further injury’.
Can core training help?
If muscle activation timing is a significant factor in LBP, an obvious question to ask at this point is whether a core training program (which often forms the staple of many a lower back injury rehab program) can help normalize muscle activation patterns? Again, there’s not much research in this area but one study is revealing(11). In this study, researchers sought to investigate activation and timing of abdominal muscle activation in response to rapid shoulder movement after an 8-week program of core stability exercises, sling exercises, or general exercises.One hundred and nine subjects with chronic LBP of at least three months' duration were randomly assigned to 8-weekly treatments with low-load core stability exercises, high-load stabilizing exercises with their shoulders in slings, or general exercises in groups. Of particular interest was the effect on muscle activation onset (recorded by ultrasound imaging) in the deep abdominal muscles in response to rapid shoulder flexion in the chronic nonspecific LBP patients.
At the end of the 8-week training period, there were only insignificant or very modest improvements in the LBP subjects, with a 15 millisecond improvement with sling training relative to core stability training, and a 19 millisecond improvement relative to general exercise training. Moreover, there was no association between changes in pain and activation onset over the intervention period. In other words, 8 weeks of core stability training produced very little improvement in the onset of abdominal muscle activation, or in symptoms.
The role of motor re-education
The evidence to date suggests that while core training may play an important role in the rehab of chronic or repeated back pain episodes, it may not be the whole answer. In a systematic review of this topic, Steiger et al reported that evidence was lacking to support the notion of treatment effects of exercise therapy in chronic LBP that were directly attributable to changes in trunk muscle strength and endurance(12). In other words, improving core muscle strength and conditioning may not be enough on its own to alleviate back pain.Furthermore, in a 2019 review of the evolution of the concepts of stability and instability relevant to back pain, researchers concluded that sufficient spinal stiffness is required to support the upper body part during dynamic activities – and that this is achieved by the fine-tuning and timely activation of the spinal muscles(13). In plain English, unless the motor recruitment patterns (timing, sequence and degree of activation) are also trained along with core muscle strength and conditioning, the benefits for back pain may be questionable.

New thinking
The growing acceptance of motor control and timing as an essential part of core training is forcing many trainers and physios to reassess the best treatment and prevention programs for chronic back pain. Moreover, research continues to show that motor control dysfunction patterns are actually quite common in athletes – even elite athletes. For example, a recent study on Olympic hockey players found over 70% of the athletes exhibited some kind of motor control dysfunction(14). And a key study published a few months ago provides further evidence that motor control training is indeed the link that has been missed by general core training, thus explaining why core training alone may fail to resolve chronic LBP. The study, which was published in the journal ‘PloS One’ investigated the correction of lumbopelvic movement and muscle recruitment patterns using motor control exercise program in people with chronic nonspecific low back pain(15).In this study, thirty adults – 15 with chronic low back pain and 15 healthy controls - were assessed using 3D motion and electromyographic analysis during repeated forward bending testing before and after a 6-week intervention program. During this 6-week period however, the 15 LBP sufferers underwent a program of training. Unlike a standard core program, this program was supervised by a physiotherapist experienced in musculoskeletal rehabilitation field, and where the program emphasized of optimal posture and re-education of faulty motor control patterns occurring in the spinal region. Training sessions lasted for 45 minutes with a ratio of 1 physiotherapist to each 5 subjects.
Each session consisted of 5-minute warm up and 5-minute cool down (stretching of the low back and thigh muscles) before and after 35-minutes of core muscle and movement control exercises using therapeutic balls and Therabands. The correct and adequate activation of the deep abdominal core muscles (namely transversus abdominus and internal obliques) of individual participants was assessed by the physiotherapist in the first session using standardized palpation (feeling for contractions) procedures(16). Any deficiencies were then targeted for correction during the practice sessions of the exercise program. The core stability and motor control exercises included:
- Hamstring roll-ins
- Hip raises
- Ball crunches
- Roll outs
- ‘Sitting marching’
- Wall squats (with the use of a therapeutic ball)
What they found
The results showed that following the core training combined with motor control training, the back pain group showed a very significant improvement in both symptoms and functional capacity – ie the ability to execute spontaneous, pain-free movements. Importantly, a 3D kinematic analysis of the movement patterns in this group found that there had been a specific motor control reorganization, producing profound and positive changes during the bending forwards activities, with the significantly enhanced activity level of lumbar multifidus and gluteus maximus (buttock) muscles.What was particularly impressive was that the chronic LBP sufferers were rehabilitated to such an extent that their performance and movement patterns became completely indistinguishable from their healthy counterparts (see figures 3 and 4). This is the first study to demonstrate that individuals with chronic LBP and compromised movement capacities are able to reset muscle activation patterns and timings sufficiently in order to return to full functional and performance capacity, with normal movement patterns – all in just six weeks!
Figure 3: Comparisons of the 1-cycle time (seconds) of the repeated bending task

Blue = healthy participants; black = chronic pain participants before the motor/core training program; white = chronic pain participants after the 6-week intervention. Faster times = improved function and more natural movement patterns. Notice the very large decrease in times following the training program.
Figure 4: Comparisons of lumbar spine and hip angular velocity during the repeated bending task

Analysis of spine and hip movement speeds in degrees per second. Again, notice the large increase in speeds in the pain group following the motor/core training program – to become indistinguishable from the healthy control group!
Implications for athletes
What do these findings mean for athletes who either are suffering from chronic back pain, or who are prone to repeated episodes of back pain (often for no apparent reason)? Well, despite our increase in understanding and the widespread take up of core training work, low back pain continues to be a significant issue among many sportsmen and women. However, more recent research on muscle activation patterns (sequence, activation levels and timing) suggests that dysfunctional motor patterns are also involved. Simply improving core muscle strength alone may not be enough if the motor patterns firing those muscles are not operating as they should.If you’re an athlete who has suffered or suffers now from chronic or repeated episodes of LBP despite performing core training on a regular basis, there’s a good chance that your muscle activation patterns are less than optimal. That being the case, your best bet is to try and find a physiotherapist or trainer who has experience in this area. It’s likely you will need to undertake some specific one-to-one training to help improve your motor patterns with the guidance and real-time input from a professional. He/she can carry out movement screening tests to help identify what motor dysfunctions may exist and how, using techniques such as biofeedback, they can be corrected. It can take a while to ‘unlearn’ incorrect muscle activation patterns that have become hardwired into your sub consciousness, but the results are likely to be very worthwhile indeed!
References
- Spine (Phila Pa 1976). 2004 Feb 15;29(4):449-54
- Neurosurg Focus. 2006 Oct 15;21(4):E7
- Br J Sports Med. 2003 Jun;37(3):263-6
- Brain Res 2001; 141:261–266
- Spine 2000; (Phila Pa 1976) 25:947–954
- Exp Brain Res 2003; 151:262–271
- Spine 2007; (Phila Pa 1976) 32:E801–E808
- Exp Brain Res 2011; 210:259–267
- J Neurophysiol. 2011 Nov;106(5):2506-14
- J Back Musculoskelet Rehabil. 2013 Apr 29. [Epub ahead of print]
- Spine (Phila Pa 1976). 2012 Jun 1;37(13):1101-8
- European Spine Journal 2012;21(4):575–98
- Journal of Orthopaedic & Sports Physical Therapy. 2019;49(6):415–24
- J Bodyw Mov Ther. 2021 Apr;26:128-133
- PLoS One. 2021; 16(11): e0259440
- “A clinical palpation test to check the activation of the deep stabilizing muscles of the lumbar spine”. International SportMed Journal. 2000;1(4)
You need to be logged in to continue reading.
Please register for limited access or take a 30-day risk-free trial of Sports Performance Bulletin to experience the full benefits of a subscription. TAKE A RISK-FREE TRIAL
TAKE A RISK-FREE TRIAL
Newsletter Sign Up
Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Keep up with latest sports science research and apply it to maximize performance
Today you have the chance to join a group of athletes, and sports coaches/trainers who all have something special in common...
They use the latest research to improve performance for themselves and their clients - both athletes and sports teams - with help from global specialists in the fields of sports science, sports medicine and sports psychology.
They do this by reading Sports Performance Bulletin, an easy-to-digest but serious-minded journal dedicated to high performance sports. SPB offers a wealth of information and insight into the latest research, in an easily-accessible and understood format, along with a wealth of practical recommendations.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Performance Bulletin helps dedicated endurance athletes improve their performance. Sense-checking the latest sports science research, and sourcing evidence and case studies to support findings, Sports Performance Bulletin turns proven insights into easily digestible practical advice. Supporting athletes, coaches and professionals who wish to ensure their guidance and programmes are kept right up to date and based on credible science.









