You are viewing 1 of your 1 free articles. For unlimited access take a risk-free trial
Athlete immunity: go with your gut feeling

Can a supplementing probiotic blend improve immune system function and protect against respiratory infections? SPB looks at new research
Regular subscribers to SPB will be aware of the link between immunity and vigorous exercise, which is something of a double-edged sword. Those who engage in regular exercise are known to have improved immune function compared to their sedentary counterparts, and indeed, exercise may even prevent or reverse the age-related decline in immunity observed in the population at large(1). However, heavy or prolonged bouts of exercise – eg running a marathon - generates a type of post-exercise immune depression sometimes referred to as ‘open window’ following the strenuous effort(2). Although this dip in immune function is transitory, it nevertheless creates favorable conditions for viruses and bacterial infections after the effort, especially in the upper respiratory tract(3). This can lead to an increase in the incidence of upper respiratory tract infections (URTIs – coughs, colds, sore throats etc) in the days following the event(3,4).Nutrition and post-exercise immunity
There’s now good evidence that nutritional strategies can mitigate the stress in the immune system generated by exercise. These strategies have long included the use of such nutrients such as protein, carbohydrate, amino acids and vitamins/minerals during and after exercise (for a more in-depth discussion, readers are advised to see this article)(5,6). In more recent years however, there’s been an increasing interest in the use of probiotic supplements for enhancing athlete immunity.As we have discussed in previous SPB articles, a growing body of research has demonstrated that the use of probiotic supplementation produces immune and gastrointestinal system benefits. These include:
- An increase in circulating leucocytes (key cellular components of the immune system)(7).
- Stimulation of the maturation of immune cells present in the gut, such as lymphocytes, macrophages, and dendritic cells(8).
- With certain strains of probiotics (eg Lactobacillus casei and Lactobacillus fermentium), a reduced risk of URTIs and flu-like symptoms, and an increase in the concentration of a key immune antibody known as ‘sIgA’ (the body’s first line of defence against pathogens) in gut mucosal tissues(9).
Probiotic formula for success
Despite the evidence for the benefits of probiotics in health (and particularly) immune function, data from studies on their effectiveness is rather variable, most likely due to fact that different studies have used different probiotic strains at different doses, and with different other components depending on the method of production of the bacteria in the supplements(10). To try and add a bit more clarity about the benefits of probiotics for maintaining post-exercise immunity and preventing URTIs following a strenuous event, a new study published in the journal ‘Nutrients’ has investigated the effects of probiotic supplementation on the production of key immune cells and subsequent URTIs after running a marathon(11).In this study, 14 healthy male marathon runners received either 5 billion colony-forming units (CFU) of a multi-strain probiotic, consisting of 1 billion CFU of each of Lactobacillus acidophilus LB-G80, Lactobacillus paracasei LPc-G110, Lactococcus subp. lactis LLL-G25, Bifidobacterium animalis subp. lactis BL-G101, and Bifidobacterium bifidum BB-G90, or a placebo for 30 days before a marathon. At the beginning of the study, the athletes’ levels of blood cytokines were measured. Cytokines are small proteins that are crucial in controlling the growth and activity of other immune system cells and blood cells. When released, they signal the immune system to do its job and help the body's immune and inflammation responses. The levels of cytokines were then reassessed 24 hours before the marathon, immediately after the marathon, and again one hour after the race (see figure 1). Blood and saliva was also tested at these same time points. All the athletes were then monitored (using questionnaires) for any URTI symptoms over the next seven days – ie to see if probiotic supplementation had actually reduced the incidence of illness post marathon.
Figure 1: Experimental design for testing and assessment

What they found
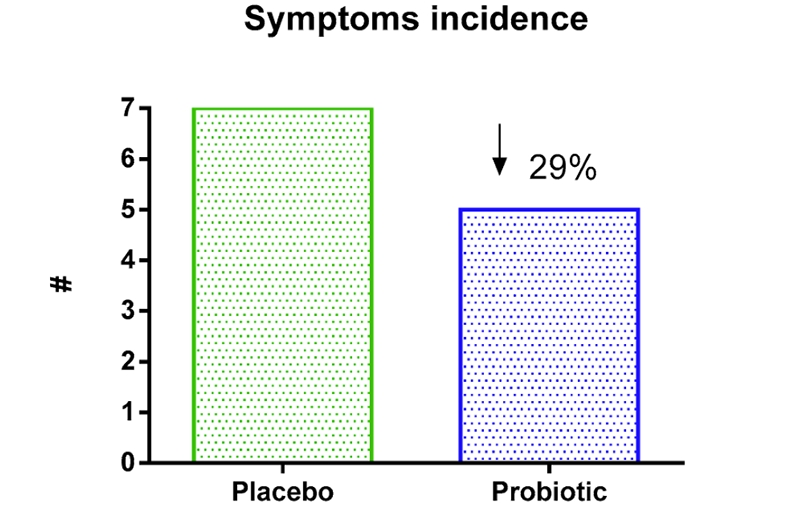
The results showed that supplementation of multi-strain probiotics was able to modulate the production of cytokines at different times and significantly decrease the incidence and severity of symptoms in the upper respiratory tracts of athletes exposed to a marathon race (see figures 2a and 2b). In particular, the probiotic group recorded lower levels of the pro-inflammatory IL-6 cytokines and higher levels of IL-10 cytokines. IL-10 is an anti-inflammatory cytokine that maintains the balance of the immune response, allowing the clearance of infection while minimizing damage to the host. In plain English, the probiotic group were able to mount a stronger and more targeted immune response after their marathon efforts than the placebo group, and this resulted in a lower incidence of URTI symptoms and severity; while both groups reported the presence of symptoms of minor infections, the incidence of URTI symptoms in the probiotic group was 29% lower when compared to placebo.Figures 2a and 2b: Symptom incidence and severity in probiotic vs. placebo athletes

Practical implications for athletes
This study provides yet more evidence for the benefits of probiotic supplementation for athletes who are seeking to maintain/improve immune function. This evidence to support this strategy seems to be quite robust when:- Athletes wish to avoid a dip in immunity/URTIs following a particularly strenuous event/training effort.
- The probiotic supplement is taken for 30 days or more before the event.
- The probiotic contains a blend of strains.
- The strength of the probiotic is standardized and adequate (at least 5bn CFUs per day in this study).
- Use bacteria strains that have proven to be effective in studies such as those mentioned above and also Lactobacillus fermentum and Lactobacillus casei.
- Probiotics in liquid form are more likely to be effective than dried forms such as capsules.
- Take any probiotic on an empty tummy and at least 15 minutes before food. A good time is soon after rising in the morning, but before breakfast.
- The beneficial changes in gut flora from probiotic supplementation takes time to accrue, which means that probiotics are not a ‘quick fix’ for boosting immunity.
- Probiotics are definitely recommended following a course of antibiotic treatment.
- Front Immunol. 2021 Apr 16;12:639308
- Sports Med. 2007, 37, 412–415
- J. Sci. Med. Sport 2010, 13, e85–e86
- J. Sports Med. 1997, 18, 91–100
- Nutr. Rev. 2008, 66, 310–320
- Exerc. Immunol. Rev. 2017, 23, 8–50
- Br. J. Sports Med. 2006, 40, 351–35
- Exerc. Immunol. Rev. 2015, 21, 70–79
- Synth. Syst. Biotechnol. 2018, 3, 113–120
- Nutrients 2017, 9, 1021
- Nutrients. 2021 Apr 27;13(5):1478
Newsletter Sign Up
Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Keep up with latest sports science research and apply it to maximize performance
Today you have the chance to join a group of athletes, and sports coaches/trainers who all have something special in common...
They use the latest research to improve performance for themselves and their clients - both athletes and sports teams - with help from global specialists in the fields of sports science, sports medicine and sports psychology.
They do this by reading Sports Performance Bulletin, an easy-to-digest but serious-minded journal dedicated to high performance sports. SPB offers a wealth of information and insight into the latest research, in an easily-accessible and understood format, along with a wealth of practical recommendations.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Performance Bulletin helps dedicated endurance athletes improve their performance. Sense-checking the latest sports science research, and sourcing evidence and case studies to support findings, Sports Performance Bulletin turns proven insights into easily digestible practical advice. Supporting athletes, coaches and professionals who wish to ensure their guidance and programmes are kept right up to date and based on credible science.











