You are viewing 1 of your 1 free articles. For unlimited access take a risk-free trial
Defend yourself with science: immune-boosting nutrients to stay well this winter
If you’re striving for a new PB, staying well could be your biggest training asset. Andrew Hamilton looks at what the recent research says about nutrition and your immunity...
In a carefully-crafted training program where you’re looking for incremental gains in performance, taking a month or even a week out due to illness can be a huge setback. The most common type of infections in sportsmen and women are upper respiratory tract infections (URTIs – coughs, colds, sore throats). Depending on the severity of an URTI, your training might be compromised for anything from a couple of days to a couple of weeks.If you’re lucky, you’ll be able to do some gentle training during an URTI, but you may find it impossible to train at all. Equally however, an infection can be more serious. A bout of influenza or a chest infection can easily result in a month or more of lost training time, which can have disastrous consequences for your fitness thanks to the process of ‘detraining’, where gains in fitness occurring as a result of training are steadily lost once training is ceased.
Given these facts, it’s natural to ask whether there are any proven ways of supporting immunity – particularly during the winter months when coughs, colds and other URTIs abound. Assuming you’re already doing the essentials (see box 1 below), let’s look at what some of the recent research says about immune-enhancing nutrients.
Box 1: Immunity – don’t forget the basics
Although the evidence for the use of particular nutrients to help support immunity is encouraging, it’s worth emphasising that at the heart of any strategy to maintain and maximise immunity is a healthy lifestyle. This involves eating a healthy diet, which should contain:- Plenty of fresh fruits and vegetables - which play a vital in promoting long-term health;
- Ample wholegrain carbohydrates (eg wholegrain breads, rice, cereals and pasta etc) - to support training;
- Sufficient high-quality, proteins (eg fresh fish, lean meats, nuts and seeds, beans, peas and lentils) to support recovery.
- Plenty of fluid to help hydrate during and after exercise;
- Only small amounts of sugary or processed (and often fatty) foods, which have little nutritional value and may actually disturb some aspects of the body’s metabolism.
Vitamin D
In recent years, the evidence that the maintenance of normal human immunity is highly dependent on the vitamin D status of individuals, and that many people (including athletes) have sub-optimum levels of vitamin D has been mounting(1). Until quite recently, there were very few specific studies on athletes, vitamin D and immunity but a large and comprehensive study published in 2013 makes fascinating reading(2).The goal of the study was to determine the influence of the athletes’ (ranging from recreationally active weekend warriors to Olympic triathletes) vitamin D status on their immune function and the incidence, severity and duration of and upper respiratory tract illness (URTI – coughs, colds, sore throats, sneezing, earaches, nasal congestion fever, chills etc) episodes over the course of a 4-month winter training period.
In a nutshell, compared with low-vitamin D status athletes, athletes with high levels of blood vitamin D had fewer episodes of URTI, less severe symptoms when they did occur and greatly improved levels of immune markers (see figure 1). Not only was this study the first to show that optimum vitamin D status in athletes undergoing vigorous training can boost immunity, it also used a large number of subjects from a range of sports, which means its findings are likely to be valid and widely applicable.
Figure 1: Vitamin D status and immunity

Subjects with high levels of vitamin D in the blood (dark grey bars) had much greater levels of cytokine (immune proteins that stimulate immune defences against bacteria and viruses) production by three types of immune cells (IL-6, IL1β and TNF-a) indicating increased immune protection. This was reflected in the fact that these subjects suffered fewer episodes of URTI during the study period.
In another study on vitamin D and athletes, researchers found that vitamin D3 inadequacy/deficiency was commonplace; some 62% of the athletes and 73% of the non-athlete controls had a blood vitamin D3 levels of less than 50nmol per litre – ie sub-optimum, deficient or severely deficient(3). These results fit with other more recent studies showing that many athletes have less than optimum levels of vitamin D in the body, with negative implications for immunity. Indeed, over the past two years alone, several studies have examined the vitamin D status of a wide range of sportsmen and women, including National Football League players(4), basketball players(5), elite swimmers(6), young female soccer players(7), elite female athletes(8), and ice-hockey players(9). In all of these studies, researchers found a high prevalence of either a sub-optimum vitamin D status (below 75 ng/ml), or an outright vitamin D deficiency (below 25 ng/ml).
Seasonality
Low vitamin D levels are particularly commonplace during the mid-late winter period, when the body’s reserves of ‘sunshine manufactured’ vitamin D during the summer months start to run low. This is because vitamin D can be synthesised from a natural substance in the body (derived from cholesterol and called 7-dehydrocholesterol) when skin is exposed to sunlight. However, it’s important to note that it’s the UVB rays in sunshine that are needed for this reaction to occur. When the sun is high in the sky, for example during summer months or all year round in the tropics, the sunlight contains sufficient UVB to enable the synthesis of vitamin D. However, when the sun is low in the sky, its rays have to pass through a greater volume of atmosphere to reach the surface, significantly attenuating the UVB content.Indeed, studies have shown that from November through to February, when human skin is exposed to sunlight on clear sunny days at latitudes of around 42oN (the same latitude as cities such as Boston, Rome and Marseilles), the UVB content of that sunshine is so low that no vitamin D can be synthesised even around midday when the sun is highest in the sky. Move up to around 52oN (for example London, Amsterdam and Berlin) and vitamin D synthesis in the skin becomes impossible from October right through to March!
Probiotics
Probiotics (for example, found in some yoghurt/yoghurt drinks) are defined as ‘live micro-organisms which, when administered in adequate amounts, confer a health benefit on the host.’ During the last fifteen years, there’s been an explosion of research into the immune boosting properties of probiotics and the results have been very encouraging. What’s been lacking until more recently however is good placebo-controlled randomised trials carried out in the field – ie on athletes engaged in their normal training programmes. To complicate matters further, numerous strains of probiotic bacteria have been used in studies, some of which may be far less effective than others. This all makes it difficult to determine just how effective probiotic supplementation for someone in hard training really is!A study looked at the effects of probiotic supplementation on the duration, incidence and severity of infections in 30 elite rugby union players who took a supplement for 4 weeks(10). During the probiotic treatment 14/30 participants never experienced a single upper respiratory tract illness or gastrointestinal episode, compared to 6/30 on the placebo supplementation (a scientifically significant reduction). Also, the number of days of illness tended to be less when the probiotic was taken.
Another study looked at Lactobacillus fermentum supplementation and gastrointestinal and respiratory-tract illness symptoms in 99 competitive cyclists(11). The cyclists were randomised to either probiotic (minimum 1 × 109 Lactobacillus fermentum (PCC®) per day) or placebo treatment for 11 weeks in a ‘double-blind, randomised, controlled’ trial – the most rigorous kind of scientific trial. At higher training loads, there was an average 70% reduction in the severity of gastrointestinal illness, which became more pronounced as training load increased. Also, the duration and severity of upper respiratory-tract illness symptoms was reduced by around 30%.
In another double-blind, placebo-controlled cross over trial study, scientists investigated the use of Lactobacillus fermentum in 20 elite male runners over a 4-month winter training season(12). Athletes taking the probiotic supplement reported less than half the number of days of respiratory symptoms during the supplementation period (30 days) compared with the placebo group (72 days). Reported illness severity was also lower for episodes occurring during the supplementation period.
In a further study, 84 athletes took either a placebo or probiotic supplement (Lactobacillus casei Shirota) for 4 months(13). The athletes taking the probiotic experienced significantly less URTIs than those who didn’t. However, to illustrate that all not all probiotics are created equal, the same scientists investigated another probiotic (Lactobacillus salivarius) on infection, cold symptom duration and severity, and immunity in 66 endurance athletes and found that it didn’t reduce the frequency of URTIs(14). In other words, it seems that if you’re tempted to use probiotics, you should try a strain for which there is good evidence in the scientific literature.
Cystine/theanine
Cystine and theanine are two amino acids that are involved in the synthesis of a compound called glutathione in the body. Glutathione helps maintain the optimum activity of very important immune cells called ‘natural killer’ (NK) cells, and recent research suggests that supplementation of these nutrients could be advantageous for immune functioning in athletes. For example, in one study, cystine (700 mg) and theanine (280 mg) were given once daily for 2 weeks to 15 men who undertook a week of normal training followed by a second week where their training load was doubled(15). In the high-intensity (2nd) week, NK cell activity declined when the men took a placebo. However, when they took cystine/theanine, NK activity was restored.In another study, 15 long-distance runners were each allocated to a cystine/theanine or placebo group and were supplemented for 10 days prior to the start of an intense training period(16). Compared to the placebo, the cystine/theanine supplement prevented a decrease in the immune function, and reduced the incidence of infection associated with the drop in immunity commonly observed after continuous intense exercise.
These results tie in neatly with the results from a 2010 study, which investigated the effects of cystine/theanine supplementation on the common cold (the most common URTI) in human volunteers(17). A total of 176 healthy male volunteers received either placebo or cystine/theanine (490 mg) tablets twice daily for 35 days. The researchers then measured the incidence of common cold symptoms using standardised and rigorously validated questionnaires. The results showed that the incidence of common cold symptoms during the trial was significantly lower in the cystine/theanine-supplemented group than in the placebo group (see figure 2).
Figure 2: Incidence of laboratory-defined colds during 35 days of cystine/theanine supplementation
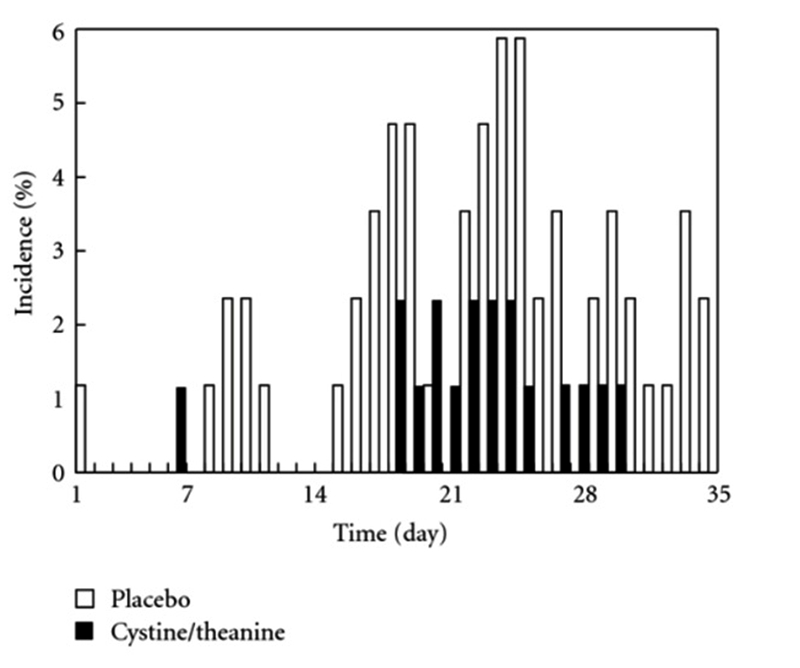
Compared to a placebo (open bars), the incidence of common colds was significantly less in the cystine/theanine-supplemented group.
Beta-glucans
Beta glucans are naturally occurring compounds (eg found in the bran of cereal grains, and some mushrooms) that can exert positive effects on the function of important immune cells. However, while there’s good evidence for the immune benefits of beta glucans in the general population, research among athletes undergoing heavy training is more limited.One double blind, placebo-controlled study investigated the effect of pleuran (an insoluble glucan from a mushroom known as Pleurotus ostreatus) on immune responses and incidence of URTIs in 50 athletes over a 3-month period(18). The results showed that the pleuran significantly reduced the incidence of URTI symptoms and increased the number of circulating natural killer (NK) cells. Since NK cells are key immune cells whose job it is to fight off viral infection, the scientists s concluded that ‘pleuran may serve as an effective nutritional supplement for athletes under heavy physical training’.
Another study looked at whether beta-glucan supplements from Pleurotus ostreatus was able to combat the temporary ‘immune dip’ that invariably occurs following a bout of high-intensity exercise(19). Twenty elite athletes took either beta-glucan or placebo supplements once a day for two months; the placebo group typically showed a 28% reduction in NK cell numbers activity during the recovery period, whereas no such reduction was found in the beta-glucan group (indicating superior immunity during the all-important recovery period!
Summary
Keeping your immunity in tip-top condition requires a multi-faceted approach, which means attending to lifestyle factors (getting enough good sleep, managing stress, eating a high-quality diet etc) and ensuring you allow sufficient recovery in your training programme, especially when the intensity increases. However, recent science suggests that certain nutrients may confer additional immune protection and these maybe useful, particularly over the winter months or during periods of high workloads.Practical implications
- Ensure your day-to-day diet contains plenty of vitamin D and is high in carbohydrate. Training while consuming insufficient carbohydrate is stressful for your body and can impair immune function;
- Consider using carbohydrate drinks during and carbohydrate/protein recovery drinks immediately after training to minimise the post-exercise dip surge in stress hormones (which suppresses immunity);
- If you suffer from frequent winter URTIs, consider taking a daily vitamin D supplement of 1000-2000IUs throughout the winter months;
- Probiotics can help support immunity but stick to those strains proven in scientific studies - eg Lactobacillus fermentum;
- If you’re particularly vulnerable to URTIs, you can consider trying cysteine/theanine and/or beta glucan supplements;
- Don’t forget good hand hygiene, which can significantly reduce your exposure to the viruses responsible for UTRIs!
References
1. Endocrinol Metab Clin North Am. 2010 Jun;39(2):365-792. Exerc Immunol Rev. 2013;19:86-101
3. J Sports Sci. 2012 Oct 22
4. J Sports Med Phys Fitness. 2018 Mar 1. doi: 10.23736/S0022-4707.18.08122-7. [Epub ahead of print]
5. Orthop J Sports Med. 2018 May 21;6(5):2325967118774329
6. Int J Sport Nutr Exerc Metab. 2017 Oct;27(5):399-407
7. Pediatr Exerc Sci. 2018 Feb 1;30(1):157-167
8. Nutrients. 2018 Jan 31;10(2). pii: E167
9. PLoS One. 2018 Apr 9;13(4):e0195284
10. J Sci Med Sport. 2013 Aug 30. pii: S1440-2440(13)00190-4
11. Nutr J. 2011 Apr 11;10:30
12. Br J Sports Med. 2010 Mar;44(4):222-6
13. Int J Sport Nutr Exerc Metab. 2011 Feb;21(1):55-64
14. Int J Sport Nutr Exerc Metab. 2012 Aug;22(4):235-42
15. J Strength Cond Res. 2010 Mar;24(3):846-51
16. Biosci Biotechnol Biochem. 2009 Apr 23;73(4):817-21
17. J Amino Acids. 2010;2010:307475
18. Eur J Appl Physiol. 2011 Sep;111(9):2033-40
19. Appl Physiol Nutr Metab. 2010 Dec;35(6):755-62
Newsletter Sign Up
Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Keep up with latest sports science research and apply it to maximize performance
Today you have the chance to join a group of athletes, and sports coaches/trainers who all have something special in common...
They use the latest research to improve performance for themselves and their clients - both athletes and sports teams - with help from global specialists in the fields of sports science, sports medicine and sports psychology.
They do this by reading Sports Performance Bulletin, an easy-to-digest but serious-minded journal dedicated to high performance sports. SPB offers a wealth of information and insight into the latest research, in an easily-accessible and understood format, along with a wealth of practical recommendations.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Performance Bulletin helps dedicated endurance athletes improve their performance. Sense-checking the latest sports science research, and sourcing evidence and case studies to support findings, Sports Performance Bulletin turns proven insights into easily digestible practical advice. Supporting athletes, coaches and professionals who wish to ensure their guidance and programmes are kept right up to date and based on credible science.













