You are viewing 1 of your 1 free articles. For unlimited access take a risk-free trial
Ankle sprains: a balanced approach to recovery

Balance and propioception training is a common rehab option for the prevention of ankle sprain injuries in athletes. But are there better options?
Ankle sprains are one of the most common musculoskeletal injuries among sportsmen and women, with some studies suggesting that up to 45% of sports related injuries may be related to ankle instability(1). Common to all ankle sprain injuries is compromised structural integrity of the ligaments, which function as joint stabilisers – most notably, the lateral ligaments (on the outside of the ankle) such as the ‘anterior talo-fibular ligament’, which is especially vulnerable to injury when the ankle ‘tips over’ (see figure 1).Figure 1: Locations of stabilizing lateral ligaments in the ankle

The three main stabilizing lateral ligaments (on the outside of the ankle) are shown here.
Causes of lateral ankle sprain
The most common single precipitating factor in lateral ankle sprain is a single-limb landing on an uneven surface – for example, when running across rutted ground(2). Another possible factor in determining the likelihood of a lateral ankle sprain is proprioception, which is an important element of the neuromuscular control. Proprioception refers to the ability of the brain to ‘sense’ where the limbs are positioned in space and time. With sufficient proprioception, an athlete landing on extremely uneven group may be able to detect the speed and magnitude of ankle perturbation in a timely fashion, and react with proper muscle activation and joint motion. However, the very nature of uneven terrain means that this is not always possible, even in athletes with excellent propioceptive skills. Moreover, the evidence for the role of propioceptive factors in precipitating ankle sprain is far from clear (as we will see later). Other factors relating to the risk of ankle sprain in athletes are shown in table 1 below.Table 1: Risk factors for ankle sprain among athletes populations(2)
Non-modifiable risk factors |
Modifiable risk factors |
| Sex | Weight |
| Age | Body mass index |
| Height | Bracing/taping |
| Race | Footwear |
| Foot/ankle anatomy | Neuromuscular control |
| Extremity alignment | Postural stability |
| Previous ankle sprain | Muscle strength |
| Generalized joint laxity | Exposure to sport |
| Player position | |
| Playing surface | |
| Skill level |
The nature of lateral ankle sprain means that once an injury has occurred, re-injury is very likely. This is because injury/damage to the lateral ligaments and joint capsule very often impairs the ability of these structures to provide optimum mechanical restraint following injury(3-10). Combined with any deficits in propioception, this means that re-injury rate following an initial ankle sprain is very common. Indeed, studies have shown that 73% of individuals who sprain their ankles are likely to experience recurrent ankle injuries(11).
Balance and propioception in lateral ankle sprain and re-injury
As mentioned above, a number of researchers have proposed that poor neuromuscular control and proprioception of the ankle joint is a significant factor in the occurrence of both initial and recurrent ankle sprains. However, despite decades of research on ankle sprain, studies have failed to find concrete evidence that subjects with ankle instability experience proprioception deficits compared to those without a history of ankle instability(12). This issue is further complicated by the fact that there is no standard testing and training protocol for ankle proprioception.For many physios and coaches, the working assumption is that that impaired proprioception and/or balance DO play a significant role in lateral ankle sprain. This is why many traditional intervention programs for the prevention and treatment of acute lateral ankle sprains and chronic ankle instability include balance and coordination training(13,14). This assumption (that impaired proprioception and/or balance play a significant role in lateral ankle sprain) is supported to a degree by research showing that balance and coordination training results in direct effects on the sensorimotor system (the system of muscle control that relies on feedback via proprioception)(15-19).
In an attempt to provide more clarity regarding proprioception, balance and ankle sprain, a comprehensive review study tried to answer the following three questions(20):
- Can preventative balance and coordination training reduce the risk of sustaining a lateral ankle sprain?
- Can balance and coordination training improve treatment outcomes associated with acute ankle sprains?
- Can balance and coordination training improve treatment outcomes in patients with chronic (ie long-term) ankle instability?
Nevertheless, these findings fit with a later study, which found that poorer neuromuscular control due to proprioception changes of the ankle joint may contribute to the high recurrence rate of lateral ankle sprain in athletes(12). In addition, it seems that after an initial injury, overstretched/loosened ligaments and/or joint capsule may hamper the function of ‘mechanoreceptors’. These mechanoreceptors are essential for propioception; any loss in their function will inhibit propioception, which would make re-injury more likely. Furthermore, it seems likely that loss of mechanoreceptor function can inhibit ankle muscle reflexes and induce ankle position sense deficits(21-25).
However, just to confuse matters further, there are also many studies that contradict these findings. For example, in studies comparing healthy and unstable ankles, no muscle reflex differences(26-28), no position sense differences(29-31), and no movement sense differences(32) were found between healthy and unstable ankles! In addition, some studies indicate that the ability to sense ankle position is NOT a good predictor for future ankle sprains(33).
Balance and strength
One the face of it, it seems as though the evidence is contradictory – ie that balance training does appear to improve the prognosis for ankle sprain and reduce re-injury rates, but that there’s little evidence that improving balance, propioception and neuromuscular control produces positive results. One possible explanation for the observations lies in the role of ankle strength; fairly recent evidence suggests that improving muscle strength could actually play a more important role in ankle sprain prevention and rehab than improving proprioception and/or balance(12).It turns out that there’s a good theoretical basis for these claims; although the impact of muscle strength on ankle stability is unclear, muscle weakness has been reported in muscles involved in controlling ankle movements when investigating ankle instability. These muscles include(34-36):
- The ankle dorsiflexors (the muscles that pull the toes up and back towards the shin).
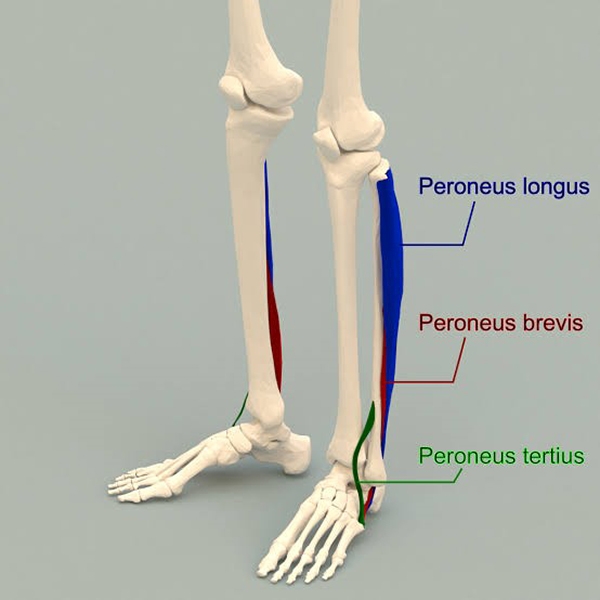
- The peroneal muscles (running from the top of the fibula near the knee] down the outer edge of the shin to the outer side of the ankle – see figure 2)
- The hip flexor muscles (muscles that raise the thighs toward the torso).
Figure 2: Location of the peroneal muscles of the lower leg
Could strength training these reduce the incidents of initial and recurrent ankle sprains by enhancing neuromuscular control of the ankle joint? This seems unlikely as strength training focuses on total activation rather than the type of activation – for example that which occurs during skills training. But what strength training may do is to help restore ankle muscle balance, position the ankle in more stable position (eg more ankle dorsiflexion tension with a stronger shin muscle function) and increase the strength of ankle ligaments. In addition, a larger/stronger muscle can also provide additional passive restraints to the ankle joint by acting as a kind of extra ‘bracing’.
It follows from the above that if balance training IS beneficial in reducing the incidents of ankle sprains, it is most likely because balance training enhances strength and stiffness in both muscles and ligaments at the ankle joint - rather than because it generates enhanced neuromuscular control. In other words, while improving neuromuscular control and proprioception at the ankle joint may be ineffective at protecting the ankle from large and fast perturbations, balance training may well increase the strength of muscles and ligaments around the ankle joint. And since ligaments are the primary stabiliser of the ankle joint, treatment protocols with a balance training component may benefit the subjects with unstable ankles.
Practical implications for athletes, coaches and physios
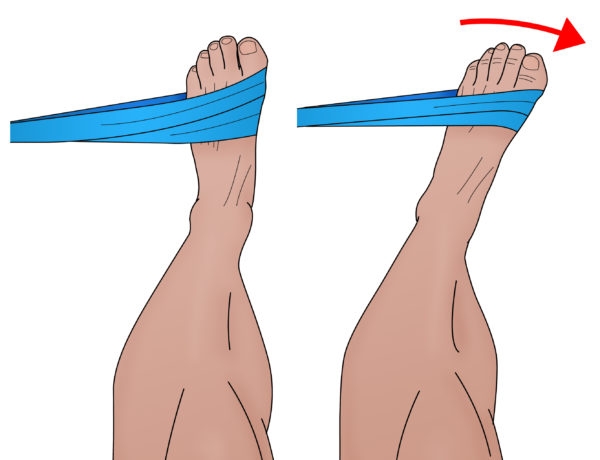
Looking at the overall evidence, what can we conclude? Firstly it seems that ankle injury prevention and rehab programs that focus purely on propioception improvement are likely to be of limited value - the evidence that propioceptive training on its own lowers the risk of initial injury or injury recurrence is quite weak. The evidence for balance training however is much stronger – although the benefits are most likely to occur as a result of improvements in muscle and ligament strength.So, although more research is needed, the evidence to date suggests that improving ankle strength may be a valuable component of any ankle injury prevention/rehab programme. Studies show that TheraBand or ankle exercises carried in all three planes of movement are effective in building ankle strength (for example, resisted dorsiflexion and plantarflexion and resisted ankle eversion and inversion – see figures 3a,b,c, and d). Indeed, one study found strength gains of 20-50% over just six weeks of an intervention program(37). Balance protocols on wobble boards can also be adapted to help develop higher levels of ankle strength – for example by holding increasing amounts of weight at progressively more elevated positions during balance training.
Figures 3a-3d: Theraband exercises to develop ankle muscle and strength
(NB, these exercises should be carried out in conjunction with general lower limb strengthening and wobble-board training with the use of increasing weights held at progressively higher positions)Figure 3a: Resisted dorsiflexion

Figure 3b: Resisted plantarflexion

Figure 3c: Resisted eversion
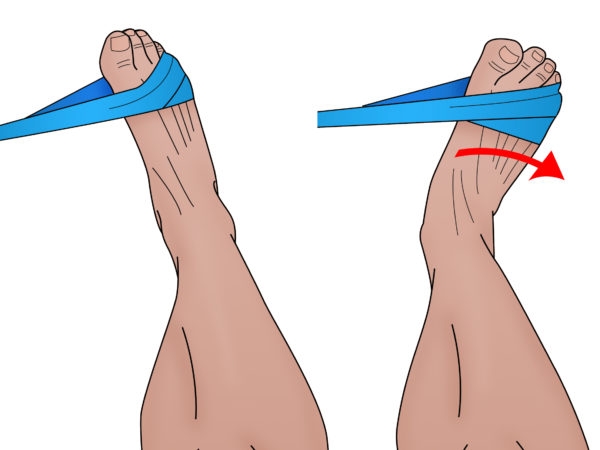
Figure 3d: Resisted inversion
References
1. Conscious Cogn 2003; 12: 609-619
2. Foot Ankle 1990; 11: 41-44
3. Aust J Physiother 2007; 53: 193-198
4. J Athl Train 2012; 47: 444-456
5. J Athl Train 1997; 32: 221-225
6. J Athl Train 2002; 37:487-493
7. J Orthop Sports Phys Ther 2003; 33:166-173
8. J Orthop Sports Phys Ther 2013; 43: A1-40
9. Am J Sports Med 2005; 33: 1174-1182
10. J Bone Joint Surg Br 1965; 47: 678-685
11. Br J Sports Med 1994; 28: 112-116
12. World J Orthop 2015 June 18; 6(5): 434-438
13. J Athl Train. 2002;37(4):413–429
14. Clin Sports Med. 2004;23(1):83–95
15. J Athl Train. 2002;37(4):364–375
16. Sports Med. 2000;29(5):361–371
17. J Athl Train. 2002;37(4):386–393
18. Med Sci Sports Exerc. 2004;36(3):388–396
19. Am J Sports Med. 2003;31(4):498–506
20. J Athl Train 2008;43(3):305–31
21. Am J Sports Med 1995; 23: 414-417
22. Am J Sports Med 1992; 20: 257-261
23. J Sci Med Sport 2010; 13: 2-12
24. Clin Biomech (Bristol, Avon) 2008; 23: 1065-1072
25. Clin Biomech (Bristol, Avon) 2014; 29: 977-983
26. J Orthop Sports Phys Ther 1997; 26: 73-77
27 Clin Orthop Relat Res 2000; (375): 193-201
28. J Athl Train 2002; 37: 475-480
29. Scand J Med Sci Sports 1999; 9: 104-109
30. Phys Ther 1987; 67:1505-1509
31. Br J Sports Med 2011; 45:660-672
32. Aust J Physiother 2007; 53: 193-198
33. Scand J Med Sci Sports 2005; 15: 336-345
34. J Bone Joint Surg Am 1955; 37-A: 1237-1243
35. Clin Orthop Relat Res 1972; 85: 50-58
36. Clin Biomech (Bristol, Avon) 2013; 28: 524-529
37. J Athl Train. 2012 May-Jun; 47(3): 282–288
Newsletter Sign Up
Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Keep up with latest sports science research and apply it to maximize performance
Today you have the chance to join a group of athletes, and sports coaches/trainers who all have something special in common...
They use the latest research to improve performance for themselves and their clients - both athletes and sports teams - with help from global specialists in the fields of sports science, sports medicine and sports psychology.
They do this by reading Sports Performance Bulletin, an easy-to-digest but serious-minded journal dedicated to high performance sports. SPB offers a wealth of information and insight into the latest research, in an easily-accessible and understood format, along with a wealth of practical recommendations.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Performance Bulletin helps dedicated endurance athletes improve their performance. Sense-checking the latest sports science research, and sourcing evidence and case studies to support findings, Sports Performance Bulletin turns proven insights into easily digestible practical advice. Supporting athletes, coaches and professionals who wish to ensure their guidance and programmes are kept right up to date and based on credible science.











