You are viewing 1 of your 1 free articles. For unlimited access take a risk-free trial
Vitamin D: Let the sunshine in!

Andrew Hamilton explains the link between vitamin D, diet, sunshine, health and performance, and why athletes almost certainly need extra vitamin D during the winter months
I still remember as a kid being force-fed cod liver oil on a teaspoon by my granny. “All that vitamin D is good for your bones and teeth!” she exclaimed as I tried not to gag. She was right of course, but it’s only very recently that we’ve begun to fully appreciate just how important vitamin D nutrition is for human health.What is vitamin D?
Before we go on to look at some of the fascinating new research on vitamin D that has been emerging of late, it’s worth taking a moment to look a little more closely at this substance. Vitamin D is actually a hormone-like substance in the body and belongs to a group of fat-soluble steroid-like compounds of which there are two major physiologically relevant forms: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D without a subscript refers to either D2 or D3 or both.Vitamin D3 is the most active form in the body and is produced in the skin of vertebrates (including ourselves!) after exposure to UVB rays from the sun. Vitamin D also occurs naturally in a small range of foods such as fatty fish, eggs, milk and some meats (table 1 below shows some good dietary sources). Your body’s ‘store’ of vitamin D therefore is a function of both your dietary intake and sun exposure.

Source: U.S. Department of Agriculture, Agricultural Research Service. USDA Nutrient Database, Release 22, 2009. ** DV = Daily Value. DVs were developed by the U.S. Food and Drug Administration to help consumers compare the nutrient contents among products within the context of a total daily diet.
A gross vitamin D deficiency, especially during childhood, can impair bone mineralisation, leading to a number of ‘soft bone’ diseases of which rickets is probably the best known. Rickets is a childhood disease characterised by impeded growth, and deformity, of the long bones(1). In the late 19th and early 20th centuries, German physicians noted that consuming 1–3 teaspoons per day of cod liver oil (rich in vitamin D) could reverse rickets, and the fortification of milk with vitamin D beginning in the early 20th century has made rickets a rare disease in Western countries such as the UK and US(2). However, it is still occasionally reported and making a growing comeback, more particularly among communities of African or Asian descent, where individuals spend a lot of time indoors and whose traditional dress covers most or all of the body(3).
Sunshine and vitamin D
Vitamin D can be synthesised from a natural substance in the body (derived from cholesterol and called 7-dehydrocholesterol) when skin is exposed to sunlight. However, it’s important to note that it’s the UVB rays in sunshine that are needed for this reaction to occur. When the sun is high in the sky, for example during summer months or all year round in the tropics, the sunlight contains sufficient UVB to enable the synthesis of vitamin D. However, when the sun is low in the sky, its rays have to pass through a greater volume of atmosphere to reach the surface, significantly attenuating the UVB content.Indeed, studies have shown that from November through to February, when human skin is exposed to sunlight on clear sunny days at latitudes of around 42oN (the same latitude as cities such as Boston, Rome and Marseilles), the UVB content of that sunshine is so low that no vitamin D can be synthesised even around midday when the sun is highest in the sky(4). Move up to around 52oN (for example London, Amsterdam and Berlin) and vitamin D synthesis in the skin becomes impossible from October right through to March!
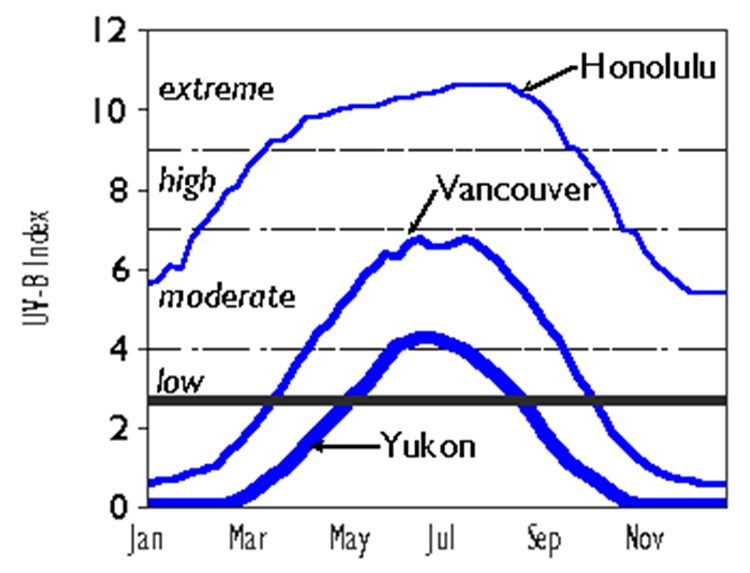
The relationship between latitude and UVB irradiation is shown in figure 1 below for three different latitudes: Honolulu at 21oN, Vancouver at 49oN and Yukon at 63oN. Note how the threshold for vitamin D synthesis (a UV index of 3 - shown by thick black line) is reached in Vancouver only from March to October an in Yukon only from May to August.
Figure 1: Latitude, UVB and vitamin D synthesis
Sunshine and health
Why is the link between sunshine and vitamin D important? Well, a number of recent studies have shown that all other things being equal, there’s a clear and linear relationship between latitude/UVB exposure and the risk of developing a number of cancers and other serious diseases such as heart disease and multiple sclerosis. For example, an Australian study found that there was an inverse association between ambient UVB radiation received by mums in the first trimester of pregnancy and subsequent risk of multiple sclerosis in the offspring(5). In short, children born in May/June (ie where the first trimester fell within the Australian summer where ambient levels of UVB are higher) were significantly less likely to develop MS than those born in November/December (whose first trimester fell within the Australian winter period) – see figure 2.Figure 2: Risk of MS

Risk of MS (solid line) plotted against month of birth overlaid with ambient UVB levels in the first trimester (dotted line). NB - UVB line is on an inverse scale – ie troughs on graph correspond to peaks in UVB.
Sunshine, vitamin D and health
Why has sunshine/UVB exposure been correlated so closely with health? Well, the evidence is now overwhelming that high levels vitamin D in the body provide significant levels of protection from a number of diseases(11). Put simply, the further away from the equator you live, the higher the risk of these diseases because your lower exposure to UVB exposure means lower levels of vitamin D in your body.The evidence emerging between higher levels of vitamin D and health is so strong that some countries such as the US have amended their guidelines on dietary vitamin D intake (see box 1) because it’s becoming very clear that the amount of vitamin D you need simply to ensure healthy bone formation is actually a long way short of the optimum intake for health.
Box 1: Updated guidelines on vitamin D intakes
In the US, new reference intakes were introduced in 2010. These are:- 1–70 years of age: 600IU per day
- 71+ years of age: 800IU/day
- Pregnant/lactating: 600IU/day
To compound the problem, there’s plenty of evidence that (especially in northern latitudes), sub-optimum vitamin D levels are widespread among the general population. For example, a German study concluded that vitamin D levels were insufficient in nearly half of the general German population and an additional 15-30% were actually vitamin D deficient – ie only a quarter of the population had adequate vitamin D levels(12).
Importantly, the researchers pointed out that adherence to present ‘sun safety’ policy (avoidance of the sun between 11 am and 3 pm) and dietary recommendations (5-10mcg daily for adults) will ‘unavoidably and definitively lead to a vitamin D deficiency’. They went on to calculate that the estimated cost savings in healthcare from improving vitamin D status in Germany might be up to €37.5 billion each year!
Vitamin D and athletic performance
So far we’ve established that plenty of vitamin D through sun exposure and dietary sources is vital to health and that sub-optimum vitamin D levels are widespread. But what are the implications for athletes? Back in the early 20th century, encouraging exposure to UVB was commonplace because many coaches and athletes believed that this was beneficial for performance despite the limited scientific evidence for this practice(13). However recent advances in molecular biochemistry have identified that human muscle tissue contains specific receptors for vitamin D and that through its action as a steroid-like hormone, vitamin D appears to be able to enhance protein synthesis (by boosting the activity of genes) within muscle tissue(14).As well as bone health, a growing body of evidence has found that optimum intakes of vitamin D in adults provide significant protection from degenerative diseases such as heart disease, multiple sclerosis and a number of different cancers(15,16). For runners in hard training however, there are other very good reasons why your vitamin D intake matters – not just for health, but for performance too:
*Immunity - A growing body of research suggests that sub-optimum vitamin D status harms immunity, but also that boosting vitamin D intake improves immunity. For example, when scientists studied 267 endurance athletes over the winter period, they found that a significantly higher proportion of those who were vitamin D ‘deficient’ came down with an upper respiratory tract infection (URTI – coughs, colds, sore throats etc) and suffered worse symptoms than those in the ‘optimal’ status group(17). Another study found that supplementing 5000IUs per day with vitamin D₃ for four weeks during the winter boosted immune function and reduced the incidence and severity of URTIs in taekwondo athletes(18). Other recent studies have provided strong evidence that 1) poor vitamin D status is linked to a higher incidence of URTIs and that 2) increasing vitamin intake, especially over the winter period, reduces the incidence and severity of URTIs(19).
*Injury risk –Vitamin D is needed for the formation of strong, healthy bones, and research clearly shows that sub-optimum intakes of vitamin D can greatly increase the risk of stress fracture in runners(20). There’s also good evidence that a poor vitamin D status increases the risk of muscle and other soft tissue injuries in athletes – particularly in the lower limbs and core muscles(21).
*Exercise performance – Some research suggests that performance might be improved in runners with an optimum vitamin D status(22) and that higher intakes of vitamin D can improve some power and strength measures in athletes(23). However, the evidence on performance is somewhat patchier, and some studies have found no benefits(24,25).
Vitamin D status
To recap briefly then, we’ve seen that vitamin D status is incredibly important for health and well being and that an optimum status is also vital for athletes. Moreover, we also know that vitamin D levels in the body are intimately linked to sunshine exposure and that those living in higher latitudes may struggle to maintain optimum levels, especially during winter months. So what does the research say about typical vitamin D levels in athletes?The evidence is not encouraging. A study by researchers from Israel looked at the vitamin D status of 98 Israeli athletes and dancers and found that no less than 73% of the subjects were vitamin D insufficient (which they defined as a blood level of less than 30 nanograms (ng) per millilitre (ml) of blood)(26). And while the insufficiency rates were higher among indoor sports, the rates for outdoor sportsmen and women were still 40%! Given that Israel is a sunny country, these results are surprising and suggest vitamin D deficiency could be even more widespread at more northern latitudes.
In a US study, researchers looked at how vitamin D levels in 41 athletes from Carolina (12 indoor, 29 outdoor) varied through the seasons(27). In addition, bone density was measured by dual energy x-ray absorptiometry, and injury and illness were documented as part of their routine care. These researchers used 40ng per ml as the cut-off for optimal status and found that, 75.6%, 15.2%, and 36.0% of athletes had an optimal status in the autumn, winter, and spring, respectively. They also found that the low concentrations in the spring were correlated with frequency of illness and recommended vitamin D supplementation during the winter to prevent seasonal decreases.
In another US study reviewing evidence on the vitamin D status of athletes(28), the researchers concluded that: “It is likely that compromised vitamin D status can affect an athlete's overall health and ability to train, by affecting bone health, innate immunity, and exercise-related immunity and inflammation.” They also argued that the optimum minimum blood levels of vitamin D for athletes need to be higher than the more conservative figure of 30-40ng per ml and recommended that athletes achieve a blood vitamin D status of at least 75ng per ml by:
- *Including regular safe sun exposure (twice a week between the hours of 10am and 3pm - ie when the sun is high in the sky) on the arms and legs for 5-30 minutes, depending on season, latitude, and skin pigmentation (see box 2);
- *When the above is not possible (eg from October to March at latitudes of 50o or more) dietary supplementation with 1,000-2,000 IU vitamin D3 per day.
Summary and practical advice for athletes
Vitamin D is far more important for health and performance than we recently believed and many nutritional researchers now believe that vitamin D deficiency is perhaps the most widespread deficiency across the globe and the cause of many diseases and early death among those who are habitually deficient. Importantly for athletes (even those who train outdoors regularly)– studies also shown that many of us, whether through diet, lack of sunshine or both, don’t get enough vitamin D with potentially serious consequences for performance.Vitamin D deficiency appears to be far more widespread than previously believed with potentially undesirable performance consequences. Athletes should therefore:
- *Aim to consume a vitamin D-rich diet all year round but especially during winter months.
- *Consider supplementation of at least 600IU per day and up to 2000IU per day in more northern latitudes during the winter months.
- *During spring, summer and autumn, try to expose the skin of the legs and arms to regular, sensible doses (5-15 minutes a day) of bright sunshine between the hours 10am and 3pm without the use of sunscreen.
- *As an additional safeguard, vitamin D levels can be checked by blood tests; athletes should ensure blood levels of at least 40ng per ml and preferably above 75ng per ml.
1. Lancet 2003;362:1389-400
2. Pediatr Int 2003;45: 509-11
3. American Academy of Dermatology. Position statement on vitamin D. November 1, 2008
4. J Clin Endocrinol Metab. 1988 Aug;67(2):373-8
5. BMJ 2010; 340:c1640
6. Professor CF. Garland. UCSD Biomedical Library lunchtime seminar series. September 26th 2008;
7. Cancer Causes Control. 2006 Oct;17(8):1091-101
8. J Epidemiol Community Health. 2008 Jan;62(1):69-74
9. Lung Cancer. 2007 Mar;55(3):263-70
10. Cancer Epidemiol Biomarkers Prev. 2011 Feb 4. [Epub ahead of print]
11. Biol Res Nurs. 2011 Jan 17. [Epub ahead of print]
12. Mol Nutr Food Res. 2010 Aug;54(8):1164-71
13. Arch Phys Med. 1945;26:641–644
14. Mol Endocrinol. 2004;18:1109–1119
15. BMJ 2014;348:g1903
16. Exerc Immunol Rev. 2013;19:86-101
17. Int J Environ Res Public Health. 2018 Sep 14;15(9). pii: E2003
18. J Nutr Health Aging. 2018;22(4):491-500
19. PM R. (2010) 2:945–949
20. Arthroscopy. 2018 Apr;34(4):1280-1285
21. Int J Environ Res Public Health. 2018 Dec 3;15(12). pii: E2724
22. Int J Environ Res Public Health. 2019 Sep 14;16(18). pii: E3422
24. PLoS One. 2018 Apr 9;13(4):e0195284
25. Nutrients. 2019 Aug 21;11(9). pii: E1960
26 Int J Sport Nutr Exerc Metab. 2008 Apr;18(2):204-24
27. Med Sci Sports Exerc. 2011 Feb;43(2):335-43
28. Int J Sport Nutr Exerc Metab. 2008 Apr;18(2):204-24
Newsletter Sign Up
Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Newsletter Sign Up
Coaches Testimonials
Dr. Alexandra Fandetti-Robin, Back & Body Chiropractic
Elspeth Cowell MSCh DpodM SRCh HCPC reg
William Hunter, Nuffield Health
Keep up with latest sports science research and apply it to maximize performance
Today you have the chance to join a group of athletes, and sports coaches/trainers who all have something special in common...
They use the latest research to improve performance for themselves and their clients - both athletes and sports teams - with help from global specialists in the fields of sports science, sports medicine and sports psychology.
They do this by reading Sports Performance Bulletin, an easy-to-digest but serious-minded journal dedicated to high performance sports. SPB offers a wealth of information and insight into the latest research, in an easily-accessible and understood format, along with a wealth of practical recommendations.
*includes 3 coaching manuals
Get Inspired
All the latest techniques and approaches
Sports Performance Bulletin helps dedicated endurance athletes improve their performance. Sense-checking the latest sports science research, and sourcing evidence and case studies to support findings, Sports Performance Bulletin turns proven insights into easily digestible practical advice. Supporting athletes, coaches and professionals who wish to ensure their guidance and programmes are kept right up to date and based on credible science.













